Strokes and Management
What I think you should known regarding the types of strokes and management
So I did a little powerpoint not long ago regarding this subject mainly because this is a subject that arises in ER on almost a daily basis. Needless to say I had a few people come up to me after the presentation saying they found the talk informative so i'm gonna share it with you. No, i'm not talking about recognizing strokes through symptoms but instead will dive into the specific types of strokes and management. Stroke cases are a big subjects when it comes to law-suits for ER physicians so the more you know about them the better. Hopefully the information below serves as a nice refresher or provides some newfound knowledge on the subject... just make sure you proof read your own CT scans (don't miss a massive brain bleed) and consult neuro.... or don't and live life on the edge... who am I to judge?
Understanding the Two Major Types of Stroke
Not all strokes behave the same way, and understanding the underlying mechanism is the key to choosing the correct intervention.
Ischemic Stroke (85% of cases)
Ischemic strokes occur when blood flow to a part of the brain is obstructed. Common subtypes include:
Large Vessel Occlusion (LVO)
A blockage in major arteries such as the internal carotid or proximal middle cerebral artery (M1). These strokes cause significant neurologic deficits and often qualify for mechanical thrombectomy.
Small-Vessel (Lacunar) Stroke
Typically caused by chronic hypertension or small-vessel disease, these strokes involve the deeper structures of the brain and may present with more isolated deficits.
Cardioembolic Stroke
A clot forms in the heart—often due to atrial fibrillation—and travels to the brain. These strokes can occur without warning and tend to be severe.
Hemorrhagic Stroke (15% of cases)
Hemorrhagic strokes result from bleeding in or around the brain.
Intracerebral Hemorrhage (ICH)
Bleeding directly into the brain tissue, often associated with hypertension, anticoagulation, or cerebral amyloid angiopathy.
Subarachnoid Hemorrhage (SAH)
Bleeding into the subarachnoid space, most commonly due to a ruptured aneurysm. Classically presents as a sudden, severe “worst headache of life.” (this is a famous line in medicine thats crucial to document in your chart)
First Priorities in the Emergency Department
Stroke management begins the moment a suspected patient enters the ED. Rapid evaluation is crucial.
Perform the NIH Stroke Scale (NIHSS)
A structured neurological exam used to quantify stroke severity and guide treatment decisions.
Identify the “Last Known Well”
Thrombolytic therapy is time dependent. The 4.5-hour window for IV thrombolytics makes this detail essential.
Stabilize with ABCs and Basic Interventions
- Airway: Intubate if GCS is below 8 or airway protection is a concern.
- Breathing: Maintain oxygen saturation above 94%.
- Circulation: Establish two IV lines, place on telemetry, and obtain an EKG.
- Glucose: Both hypoglycemia and hyperglycemia can mimic or worsen stroke.
- Just want to point out that I have personally seen many people with low blood sugar that have been stroke alerted... just know that getting a fingerstick glucose should be one of the first things that happens upon arrival.
- Temperature: Treat fever promptly to minimize ischemic injury.
- Exposure: Check for contraindications or clues such as medication patches.
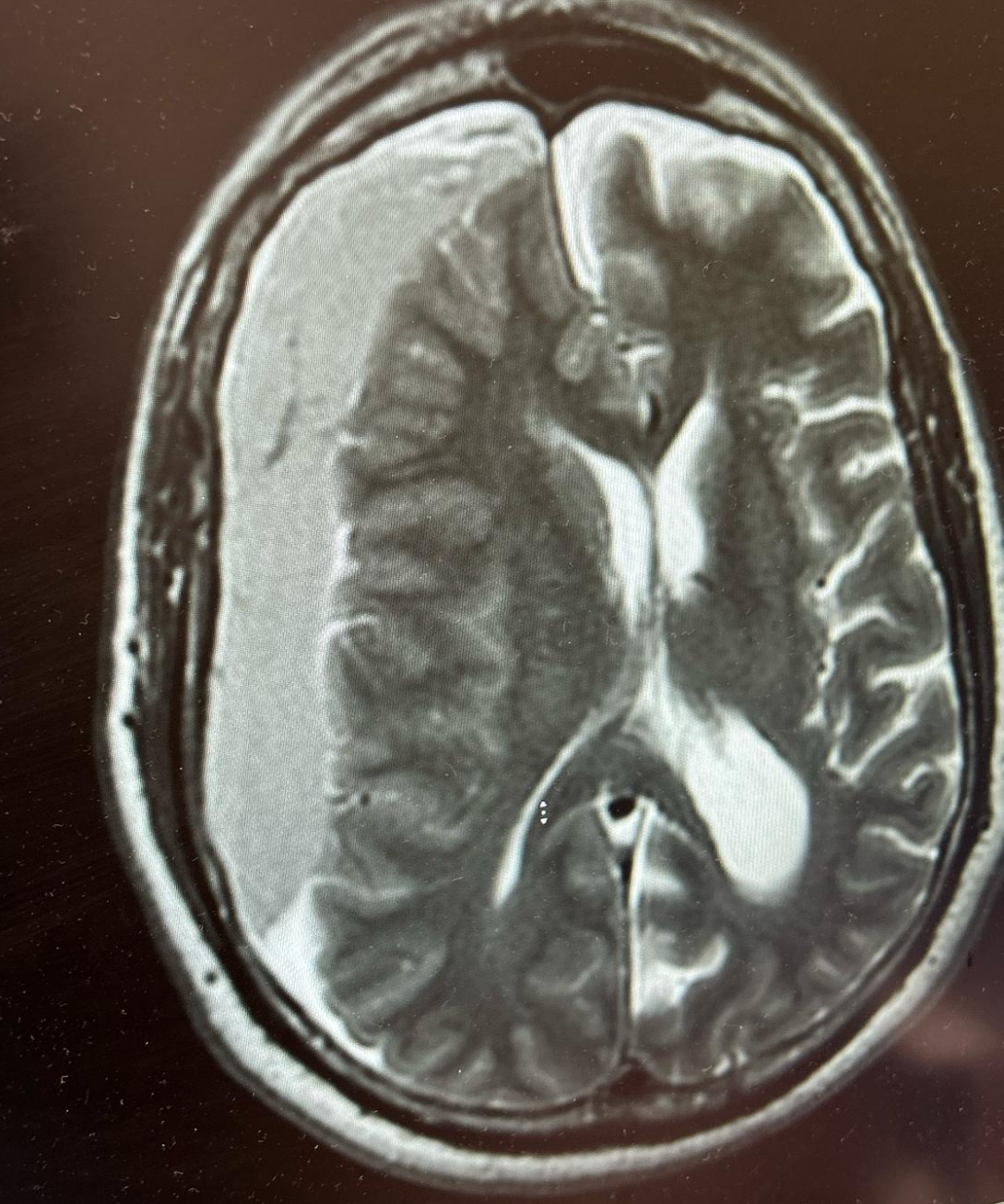
Imaging: The Foundation of Stroke Decision-Making
Rapid imaging guides nearly every clinical decision in stroke care.
Non-Contrast CT
The first and most critical imaging step. Its primary purpose is to rule out hemorrhage. It also allows calculation of the ASPECTS score, a measure of early ischemic changes.
- ASPECTS score <= to 5 generally has poor outcomes, CT perfusion must be done to see if anything can be salvaged.
- ASPECTS score between 7-10 tends to be good!
CT Angiography
Determines whether an LVO is present, guiding decisions about mechanical thrombectomy.
CT Perfusion
Used when evaluating whether a patient outside the traditional window may still benefit from thrombectomy based on salvageable brain tissue.
Management of Ischemic Stroke
Intravenous Thrombolytics (tPA or Tenecteplase)
Eligible patients should receive thrombolytics within 4.5 hours of symptom onset. Blood pressure must be controlled to:
- <185/110 mmHg before tPA
- <180/105 mmHg after tPA
Aspirin is deferred for 24 hours after thrombolytic administration.
For minor strokes (NIHSS <3), dual antiplatelet therapy—aspirin plus clopidogrel—may be recommended for 21 days.
Mechanical Thrombectomy
Indicated for LVOs.
- Most effective within 6 hours.
- Can be performed up to 24 hours in select patients with favorable perfusion imaging.
- This is the reason many hospitals call "stroke alerts" within 24 hours from symptom onset
Thrombectomy is one of the most game-changing interventions in modern stroke care.
Supportive Care Essentials
- Elevate head of bed to >30 degrees.
- Maintain euvolemia.
- Keep glucose under 180 mg/dL.
- Initiate DVT prophylaxis when appropriate.
- Ensure a swallow evaluation before oral intake.
- Engage early rehabilitation for functional recovery.
Management of Intracerebral Hemorrhage
Blood Pressure Control
Target a systolic range of 140–160 mmHg. Preferred agents include nicardipine and labetalol.
- Nicardipine (Cardene is brand name): generally dose is 5 mg/hr up to 15 mg/hr
- generally adjust by 2.5 mg/hr every 5-15 minutes
- favorable for continuous control
- Labetalol: bolus 10-20 mg IV over 1-2 minutes. Continous dose is 0.5-2 mg/minute but this is less common practice than the above.
- Can redose every 10 minutes
- Max cumulative dose 300 mg
Reversal of Anticoagulation
- Warfarin: PCC plus vitamin K
- Factor Xa inhibitors (apixaban, rivaroxaban): Andexanet alfa
- Dabigatran: Idarucizumab
Rapid reversal reduces hematoma expansion.
When to Consult Neurosurgery
Realistically you are going to consult neurosurgery for practically every brain bleed... but do it fast if you see:
- Large lobar hemorrhages
- Cerebellar hemorrhages >3 cm
- Significant mass effect (>15 mL volume or >5 mm midline shift)
Intracranial Pressure Management
- Elevate head of bed
- Use mannitol or hypertonic saline as appropriate
- Intubate if there is declining mental status or airway compromise
Hyperosmolar Therapies: Mannitol vs Hypertonic Saline
Mannitol
An osmotic diuretic that decreases brain swelling by drawing water into the intravascular space.
Avoid serum osmolarity above 320 mOsm/kg. Typical dosing is 0.25–1 g/kg every 4–6 hours.
Hypertonic Saline
Improves cerebral perfusion pressure without diuresis, making it ideal for hypotensive or volume-depleted patients.
Target serum sodium 145–155 and osmolality 300–320.
Subarachnoid Hemorrhage: Aneurysmal Emergency
Diagnosis
Begin with non-contrast CT. If findings are negative but suspicion remains, perform a lumbar puncture. CT angiography is required to identify aneurysms.
- CT non-contrast is best in 6 HOURS! (sensitivity is around 98-99%)
- If >6 hours consider doing an LP
- You will get Xanthochromia which becomes more obvious towards the 12 hours mark after symptoms begin as the red cells break down to produce bilirubin. You also get relatively consistent red cells across tubes. You may also get elevated opening pressure.
Management Principles
- Maintain systolic blood pressure below 140 mmHg.
- Administer Nimodipine every 4 hours to prevent vasospasm.
- Recognize classic features, including sudden severe headache, photophobia, and neck stiffness.
Key Stroke Metrics Every Team Should Know
- Door to CT: under 20 minutes
- Door to thrombolytics: under 60 minutes
- Door-to-groin (thrombectomy): under 90 minutes
Understanding Outcomes of tPA
Among 100 patients treated:
- 32 experience meaningful improvement
- 6 develop symptomatic ICH (bleed) but no increases in mortality at 3 months
- 1–2 suffer fatal hemorrhage
Still, thrombolytics remain a cornerstone therapy, increasing functional independence at three months by approximately 12% per the NINDS trial. Also per this trial the number needed to treat is around 8
So there you have it. A read that summarizes what I think is the crucial things to know regarding strokes. Make sure to always document well in your chart and when discussing risks and benefits of thrombolytics with patients, you can use the facts pulled from the NINDS trial. Also be sure to look up who can't have thrombolytics because there is a longggggg list.
References:
Powers WJ et al. (2019). Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines. Stroke. 50:e344–e418.
Berge E et al. (2021). European Stroke Organisation (ESO) Guidelines on Intravenous Thrombolysis for Acute Ischaemic Stroke. European Stroke Journal. 6:I–LXII.
NINDS rt-PA Stroke Study Group. (1995). Tissue Plasminogen Activator for Acute Ischemic Stroke. New England Journal of Medicine. 333:1581–1587.
Hacke W et al. (2008). Thrombolysis with Alteplase 3 to 4.5 Hours After Acute Ischemic Stroke (ECASS III). New England Journal of Medicine. 359:1317–1329.
Hacke W et al. (2004). Association of Outcome With Early Stroke Treatment: Pooled Analysis of ATLANTIS, ECASS, and NINDS rt-PA Trials. Lancet. 363:768–774.
Emberson J et al. (2014). Effect of Treatment Delay, Age, and Stroke Severity on the Effects of Intravenous Thrombolysis With Alteplase: Individual Patient Data Meta-analysis. Lancet. 384:1929–1935.
Mendelow AD et al. (2005). Early Surgery Versus Initial Conservative Treatment in Spontaneous Supratentorial Intracerebral Haemorrhage (STICH). Lancet. 365:387–397.
Tintinalli JE et al. (2016). Tintinalli's Emergency Medicine Manual, 8th Edition. McGraw-Hill.



